Julie Doniere, MD
Julie Doniere, MD
WACEP Board of Directors
I know… another article about opiates. Bear with me, I am writing this because I am anxious to start some conversations about treatment of opiate abuse. Specifically, I am eager to hear about what is happening in the ED’s across Wisconsin.
In my practice, I feel like the biggest challenge is finding treatment for those patients that are seeking help with their opiate abuse. Current practice is often symptomatic treatment, a referral list, and a “good luck!” We see people at their most vulnerable. We are either taking care of them after overdose, identifying their abuse disorder by looking at old charts, or being there when they realize they have a problem and present themselves to the ED.
There are some caveats to opiate treatment. Opioid addiction does not respond to the same treatments as alcoholism. Abstinence therapies do not typically work. These patients have a desperate need to avoid withdrawal.
This is where buprenorphine can be helpful. While incorporating bup into my treatment in the ED, I have encountered multiple misconceptions about the drug:
Myth #1: You can’t administer Buprenorphine in the ED without an X-Waiver.
BUSTED: Any ED physician or midlevel provider can use buprenorphine in the ED to treat opiate withdrawal. The patient can return to the ED for 3 days In a row to get buprenorphine.
Myth #2: Buprenorphine is a scary drug and will throw my patient into withdrawal.
BUSTED: Well, kind of busted. Buprenorphine will cause withdrawal symptoms. It should be given only to that subset of patients who are already in withdrawal; the COWS scale can measure this, I use MDcalc. When a patient has a COWS scale of 8 or greater, buprenorphine can be given.
Myth #3: Every opiate addicted patient in the county will be inundating my ED for buprenorphine.
BUSTED: ED’s that have initiated buprenorphine have seen a decline on drug seeking behavior.
Myth #4: We are trading one addiction for another.
BUSTED: The goal of medical assisted treatment is to trade addiction for dependency. Abstinence from opiates is the goal. While buprenorphine is an opiate agonist, it works primarily to control withdrawal symptoms so that individuals have more control over their cravings and avoid the risky use of opiates.
By no means is this article meant as a fully informative review of buprenorphine in the ED. I am not smart enough for that! If you are interested in a deeper dive into the role of buprenorphine in the ED, please view one of these two webinars:
- Developing an ED Initiated Buprenorphine Program (View)
- Buprenorphine 101 - Demystifying Medication Assisted Treatment in Wisconsin (View)
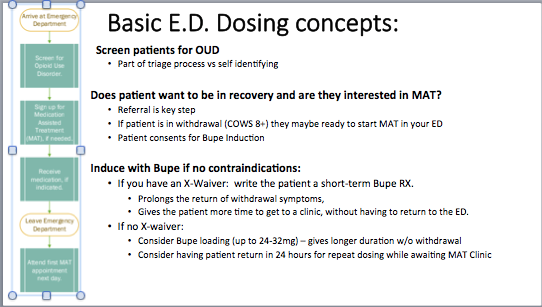
The following information about ED dosing concepts is thanks to Dr. Donald Stader, an ED doc in Colorado: